When Language Access is Prioritized, Everyone’s Care Improves
When it comes to health care, we all want to be able to access the care we need, communicate with ease, and leave with a clear understanding of what comes…
 When Language Access is Prioritized, Everyone’s Care Improves
When Language Access is Prioritized, Everyone’s Care Improves
When it comes to health care, we all want to be able to access the care we need, communicate with ease, and leave with a clear understanding of what comes…
 TrumpRx: A Smoke Screen, Not a Solution
TrumpRx: A Smoke Screen, Not a Solution
President Trump recently unveiled “TrumpRx” — an initiative touted as a major step toward lowering prescription drug prices. But peel back the packaging, and it’s clear this isn’t the sweeping…
 Unpacking The Big Bad Bill’s Impact: What It Means for Black Health and Wealth
Unpacking The Big Bad Bill’s Impact: What It Means for Black Health and Wealth
At the Congressional Black Caucus Foundation’s Annual Legislative Conference (#ALC54), Community Catalyst convened a powerhouse panel to unpack the urgent health and economic consequences of President Trump and congressional Republicans’…
 The Clock Is Ticking: New Medicaid Changes Could Strip Away Care When People Need It Most
The Clock Is Ticking: New Medicaid Changes Could Strip Away Care When People Need It Most
When faced with a medical crisis, the last thing you should have to worry about is navigating unnecessary bureaucratic hurdles. But a looming new health care law, included in the…
 Wall Street Sued an Insurance Giant to Deny More Health Care and Boost Their Bottom Line; Voters Want a System That Puts People Over Profit
Wall Street Sued an Insurance Giant to Deny More Health Care and Boost Their Bottom Line; Voters Want a System That Puts People Over Profit
When Wall Street speaks this plainly, we should all pay attention. In a new lawsuit filed last month, UnitedHealth Group investors revealed what too many families already know: the business…
 Grassroots Power Saved Health Care in Indiana—We Need It Everywhere Now
Grassroots Power Saved Health Care in Indiana—We Need It Everywhere Now
In January 2025, Indiana lawmakers introduced Senate Bill 2, a proposal backed by the billionaire-funded Foundation for Government Accountability (FGA) that threatened to upend the state’s Medicaid program. The bill…
 A Moment of Reckoning—and Possibility
A Moment of Reckoning—and Possibility
Polling tells us voters are ready to rebuild health care from the ground up; looming cuts tell us policymakers aren’t listening. Community Catalyst CEO Linda Goler Blount explains how we…
 Your health insurance could cost 20% more next year—here’s why
Your health insurance could cost 20% more next year—here’s why
Insurers are warning of the biggest premium hikes in a decade. Why? Because Congress is gutting health care to fund tax breaks for the wealthy. The numbers are in and…
By Orla Kennedy, Community Catalyst; Deborah Steinberg, Legal Action Center; and Lindsey Vuolo, Partnership to End Addiction One in three people knows someone who has died from a drug overdose….
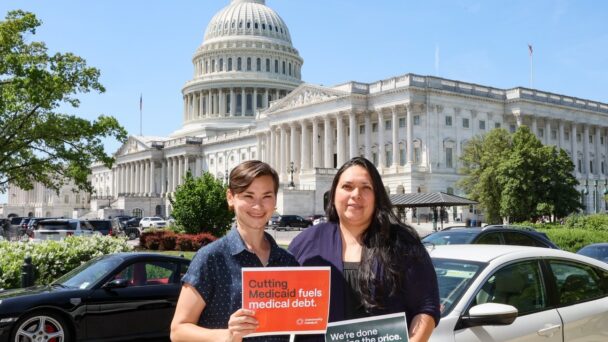
 The Big Bad Bill: What You Could Lose Overnight
The Big Bad Bill: What You Could Lose Overnight
Behind the slogans, the reconciliation bill is a direct attack on our care. Imagine waking up to find your coverage gone, your hospital closed, or your medical bills soaring. That’s…
Let’s unite for health justice. Together, we’ll work toward a more just and equitable health system.
Take Action